- About the Joint Research Network


The Joint Research Network was established in 2007. As part of on-going development of maternity care services within the National Maternity Hospital (NMH) the Director of Midwifery and Nursing recognised that research links between the NMH and their education partners, University College Dublin, School Of Nursing, Midwifery and Health System should be formalised. The Joint Research Network was established by Mary Brosnan and Professor Michelle Butler to develop a research culture for midwives, student midwives and nurses. The vision and goals of the group were to translate evidence-based midwifery and nursing knowledge into practice. Since 2007, the group has expanded and evolved to include our Ireland East Hospital Group partners.
JRN Philosophy
Midwives, Nurses, Academics and Students Working Together in a Community of Practice and Research
Membership
Academics from UCD School of Nursing Midwifery and Health Systems.
Midwifery and nursing staff and students in the Ireland East Hospital Group.
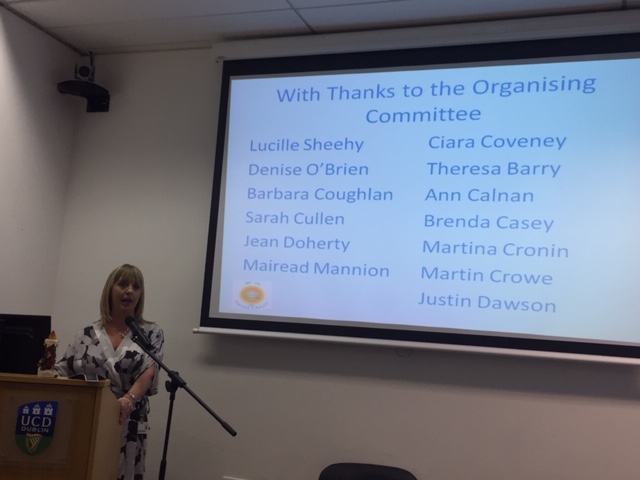
National Maternity Hospital, Chair: Lucille Sheehy
University College Dublin, Chair: Dr Denise O’Brien
National Maternity Hospital, Vice Chair: Sarah Cullen
University College Dublin, Vice Chair: Dr Barbara Coughlan
Chairs and Vice Chairs at The Joint Research Conference, December 2017

Founding members
Professor Michelle Butler, Executive Dean for Health and Science Dublin City University Dublin.
Mary Brosnan, Director of Midwifery, National Maternity Hospital
- Schwartz rounds
Working in a busy maternity hospital is a very rewarding and usually joyful experience for staff. However, it can also be stressful and emotionally difficult work. Both clinical and non-clinical staff deal with emergency situations, critically ill patients and also the death of a baby during pregnancy or after birth on a regular basis. Being involved in these situations can cause feelings of profound sadness, stress and self-doubt for staff. Schwartz rounds provide staff with an opportunity to reflect on the emotional impact of their work and support each other. Schwartz Rounds have been shown to support staff in their work and increase their empathy and compassion for colleagues and patients.
Schwartz rounds were commenced in September 2019 and are held every 5-6 weeks. Due to Covid-19 rounds are now held virtually.
The evaluation of Schwartz rounds is now complete, the full report is available here.
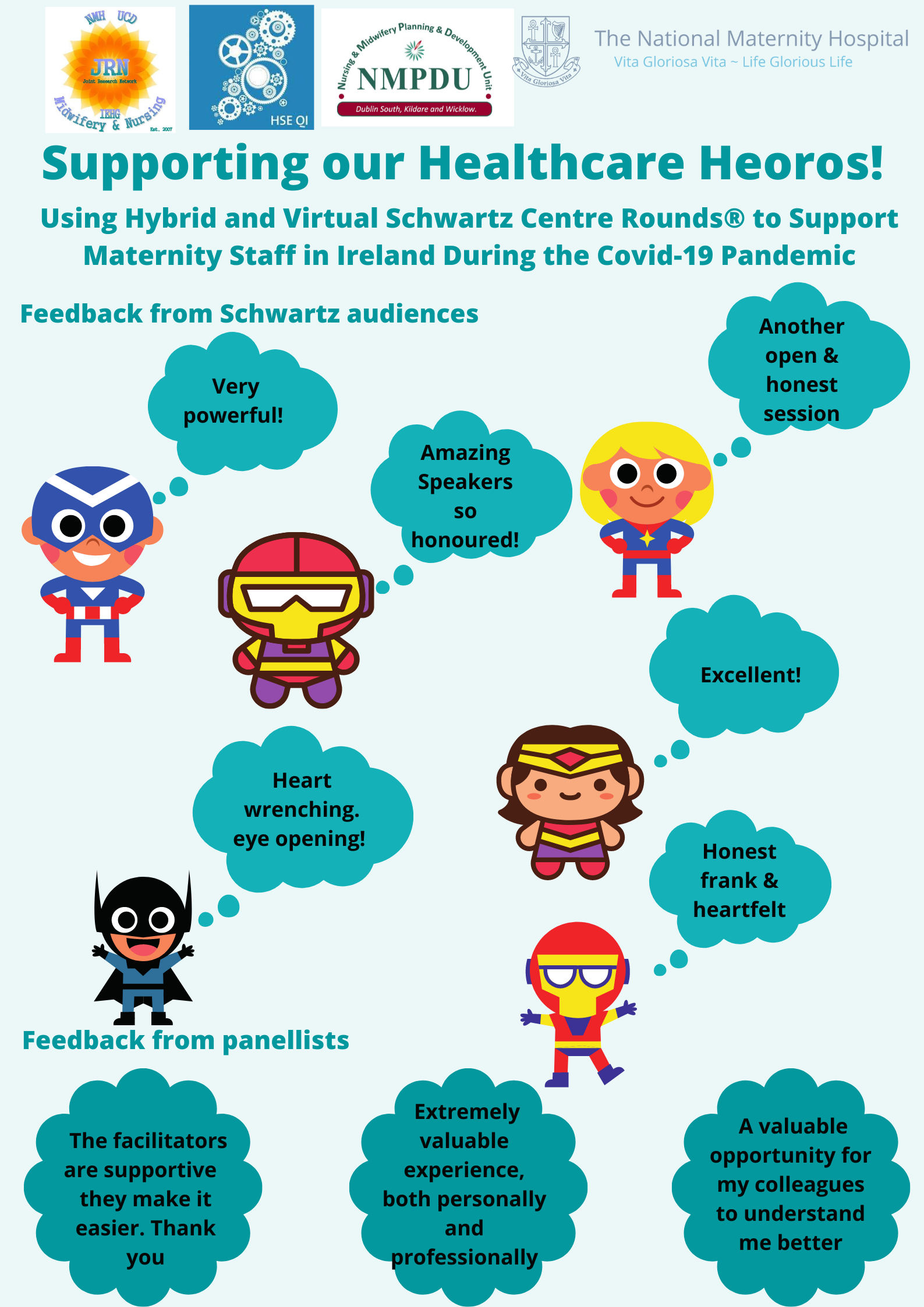
The evaluation of Schwartz Rounds is now published in the Journal of Nursing Practice and can be found here
Further information about our experience of implementing Schwartz Rounds can be found in the Irish Journal of Medical Science here
Further information about Schwartz Rounds can be found on the HSE website here
- Diabetes in Pregnancy
- Labour Hopscotch

In response to rising intervention rates, a community midwife working within the DOMINO and home birth services designed and produced a framework entitled ‘Labour Hopscotch’ in 2015 which supports both normal physiological birth and evidence-based midwifery practice. To ascertain the benefits that can be gained for women that use the Labour Hopscotch framework during childbirth, an evaluation was conducted. The study was conducted over an 18-month period commencing in September 2016, the study design is a mixed-method approach utilising an outcome survey instrument and focus group meetings to obtain data. The survey design included several open-ended questions and offered participants an opportunity to provide detailed accounts of their experiences. Following the pilot study, which included 100 participants, an output evaluation survey was conducted with 809 completed responses returned in 2017. Following the survey, a focus group meeting was held with midwives in 2018 to evaluate their experiences of the processes involved in the current implementation and provision of the Labour Hopscotch framework in the NMH.
In total 94% of participants stated they found the Labour Hopscotch useful, 72% of participants reported they were confident or very confident to stay home and utilise the Labour Hopscotch to cope with early labour. 79% of women were supported throughout the stages of the Labour Hopscotch framework during childbirth by their birth partner. 40% of participants stated the Labour Hopscotch framework influenced their decision-making around pain relief methods during childbirth. Choice of model of care, type of birth, and age were significantly associated with receiving an epidural. Midwives find the Labour Hopscotch useful as a framework to support women during childbirth.
- Bereavement Research
Bereavement Research
The bereavement research team (sub group of the JRN) have completed 3 research projects to date. Further information about the findings of these studies can be found in the publications listed below
An exploration of the prevalence and patterns of care for women presenting with mid-trimester loss.
This study aimed to explore the prevalence and patterns of care for women with MTL in a large Maternity hospital in Ireland. A descriptive, exploratory study was used involving a retrospective chart audit. 220 women presented with MTL over the 3 year data collection period. Results suggest the incidence of mid-trimester loss may be slightly lower than the 1 or 2% of pregnancies reported in the literature. Results also highlight the pain relief used, the follow up care provided and lead to the development of our second study which examined parents’ experience of care.
An Exploration of Mothers’ and Fathers’ Experiences of Hospital Care During Second Trimester Miscarriage in the National Maternity Hospital.
The aim of the study was to explore parents’ experiences of hospital care during a second trimester miscarriage. This study aimed to report on parents’ experiences of services from the time of diagnosis of the second trimester miscarriage through to follow up care received. A focused ethnographic design was used to complete this study. A series of semi-structured interviews were completed with 14 bereaved parents (9 mothers and 5 fathers). Two Global Themes emerged from the data collected from bereaved parents these included; Clinical Care Needs and Relational and Social Experiences of Miscarriage. Physical Care Needs highlighted parents’ experiences in relation to medical care, hospital facilities and information.
Full report is available here
Bereavement Care Education and Training in Clinical Practice: Supporting the development of confidence in 4th year BSc Midwifery and Higher Diploma Midwifery students in the National Maternity Hospital.
A one-day interactive Educational Training Workshop in Bereavement Care (ETWBC) was developed for student midwives in a Dublin Maternity Hospital. This workshop was then evaluated. A mixed methods design was used. 38 students completed two questionnaires at three-time intervals: pre and post-workshop, and at 3month follow up. Qualitative information was then collected to evaluate the experience for students of participating in the workshop and discuss their future bereavement care needs, using two focus groups. The results of this study suggest that all BSc Midwifery and Higher Diploma Midwifery curricula would benefit from having such an interactive workshop to increase students’ confidence in the delivery of effective bereavement care. The content of this workshop can be utilised in any maternity setting in Ireland and is recommended, not only for the midwifery cohort but all staff members looking after parents suffering perinatal bereavement or pregnancy loss.
Full report is available here
Publications
The team has disseminated the research findings and methods used through oral and poster presentations at National and International conferences focusing on Maternal and Infant Health Care. Below is a list of published peer reviewed papers on the above research studies;
Doherty, J., Coughlan, B., Casey, B., Llyod, B., Sheehy, L., Brosnan, M., Barry, T., McMahon, A. and Cullen, S. (2018) Student midwives’ education needs and their experiences of attending a bereavement education workshop. British Journal of Midwifery, 26(8):523-531 https://doi.org/10.12968/bjom.2018.26.8.523
Doherty, J, Cullen, S., Casey, B., Llyod, B., Sheehy, L., Brosnan, M., Barry, T., McMahon, A. and Coughlan, B. (2018) Bereavement care education and training in clinical practice: supporting the development of confidence in student midwives. Midwifery. 66, 1-9 https://doi.org/10.1016/j.midw.2018.06.026
Cullen, S., Coughlan, B., McMahon, A. Casey, B., Power, S. and Brosnan, M. (2018) Parents’ experiences of clinical care during second trimester miscarriage. British Journal of Midwifery 26(5):309-315 https://doi.org/10.12968/bjom.2018.26.5.309
Cullen, S., Coughlan, B., Casey, B., Power, S. and Brosnan, M. (2017) Exploring parents’ experiences of care in an Irish hospital following second-trimester miscarriage. British Journal of Midwifery, 25(2):110-115 https://doi.org/10.12968/bjom.2017.25.2.110
Cullen, S., Power, S., Coughlan, B., Chaney, J., Butler, M. And Brosnan, M. (2016) An exploration of the prevalence and patterns of care for women presenting with mid-trimester loss. Irish Journal of Medical Science. 186(2):381-386 https://doi.org/10.1007/s11845-016-1413-y
- The Perineal Management Study
Perineal Management Study: Exploring Midwives Clinical Practice and Professional Development.
In this study data was collected on current clinical practice in relation to perineal management, to explore the clinical decisions made by midwives regarding perineal management during the second stage of labour and to seek midwives’ input on perineal management education. Lack of clear evidence-based guidelines, in relation to perineal management, appeared to affect midwives’ confidence in perineal management. The need for the development of an education programme for midwives which focuses on methods to reduce perineal trauma was reported and is now being developed by the research team.
The first paper based on this study is now published in 'Midwifery', see link below
https://www.sciencedirect.com/science/article/pii/S0266613820301893?via%3Dihub
- The Latch On Study
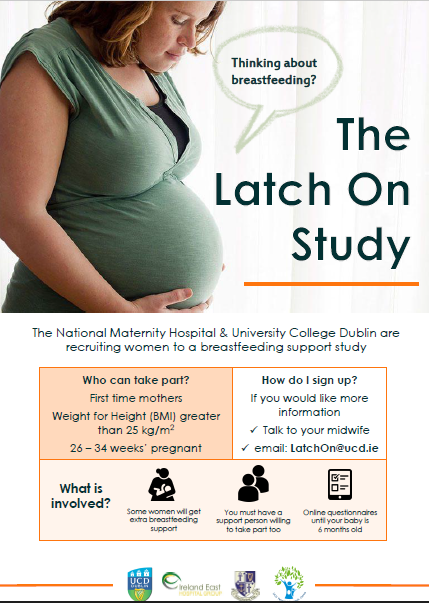
LatchOn: A multi-centre, randomised controlled trial of perinatal support to improve breastfeeding outcomes in women with a raised BMI >25
Breastfeeding rates in Ireland are among the lowest worldwide. At hospital discharge, 60% of infants are being breastfed, with only 50% exclusively breastfeeding. At 3 months of age, 35% are fed any breastmilk. Women with a high BMI are at increased risk of poorer breastfeeding practices, with lower initiation rates and duration of breastfeeding observed. This is a particular concern in Ireland, given than 50% of women have a BMI of >25 kg/m2 at their first antenatal appointment.
This is a multi-centre, randomised controlled trial of perinatal breastfeeding support among women with a BMI >25 kg/m2, using a previously-tested, multi-component intervention.The primary outcome is any breastfeeding at 3 months. Women during a first pregnancy and with a BMI >25 kg/m2 are invited to participate.The intervention will target mothers and their support partners and spans the perinatal period from late pregnancy to six weeks postpartum.
Intervention components include:
- Group antenatal education for prospective mothers and their support partners
- Individual education in the immediate postnatal period
- Professional support to six weeks postpartum and weekly phone calls in the postpartum period from an International Board Certified Lactation Consultant.
Further enquiries can be directed to: latchon@ucd.ie
- The POPPY Study
In 2013, a postnatal morbidity clinic, called the Poppy clinic, was developed by a senior midwife and consultant obstetrician. The clinic provides a service for women who experience a morbidity in the antenatal, intrapartum or postnatal period. Examples of these include wound breakdown or infection, post-partum haemorrhage, obstetric anal sphincter injury or traumatic birth requiring debriefing. As the clinic continues to grow, the clinical team deemed it imperative to evaluate the clinic to gain feedback on women’s experiences of attending the clinic, and ideas from the women who attend the clinic on how the clinic could be improved?
- Irish Health Care Centre Awards 2019
We were shortlisted under the category of ‘Best Research Paper of the Year’



We attended the awards ceremony on the 24th of September and were delighted to win the award
This was a joint application for 3 research projects.
Study 1 Perineal Management Study: Exploring Midwives Clinical Practice and Professional Development.
The level of morbidity associated with perineal trauma during birth emphasises the need to find ways to prevent or reduce it as much as possible. In this study data was collected on current clinical practice, to explore the clinical decisions made by midwives regarding perineal management during the second stage of labour and to seek midwives’ input on perineal management education.
Lack of clear evidence-based guidelines, in relation to perineal management, appeared to affect midwives’ confidence in the perineal management. The need for the development of an education programme for midwives which focuses on methods to reduce perineal trauma was reported. Content and teaching strategies will be included in a new educational programme for perineal management in 2019.
Study 2: A Study to Evaluate the Outcomes from the Implementation of the Labour Hopscotch Framework

The rates of caesarean section are increasing, reflective of international trends in contemporary maternity care. These rates are occurring in conjunction with international concerns that societal confidence for physiological labour is declining. As a response, a framework entitled ‘labour hopscotch’ was designed which supports both normal physiological birth and evidence-based midwifery practice.
94% of participants found the labour hopscotch useful, 72% of participants reported they were confident to stay home and utilise the Labour Hopscotch in early labour. Midwives, student midwives and partners also found the labour hopscotch a valuable framework to support women during childbirth. Epidural rate was 39% which is significantly lower than the annual hospital rate of 68.4% in 2017. 40% (n=309) of participants reported it had influenced their decision-making about pain relief.
Study 3: Student Midwives’ Education Needs in Relation to Bereavement Care
Student midwives and newly qualified midwives often report a lack of confidence in communicating with grieving parents. This led to the development of a Workshop on Bereavement Care focusing on the needs of students to build confidence in clinical practice. The workshop included practical advice for students about communication; making memories; parents’ perspectives on the impact of bereavement and included the use of simulation and role-play.
The workshop was positively evaluated by the student midwives and the role plays were deemed the best part of the day. Participation in the workshop increased student midwives’ confidence and self-awareness to provide bereavement care and is now integrated into the Midwifery Curriculum in UCD. Future experiential learning development using role plays will include collaboration from Support Groups. Opportunities to modify the workshop for multi-disciplinary teams are currently being explored.
- Joint Research Network Conference 2018
The conference was a showcase of the collaborative research outputs from the past 11 years.
Recent midwifery and nursing research project findings and outputs from the group were presented. Prof. Sarah Kenyon Institute of Applied Health Research University of Birmingham and Prof. Declan Devane NUI Galway, Director of the Health Research Board - Trials Methodology Research Network (HRB-TMRN), were the key note speakers discussing developing clinical research and changing practice. The conference was attended by 78 healthcare professionals from all around the country.
The conference booklet can be downloded here